
Gut Health Improvements Linked to Probiotic Use in Chronic Kidney Disease
Greg Howard
4th June, 2024
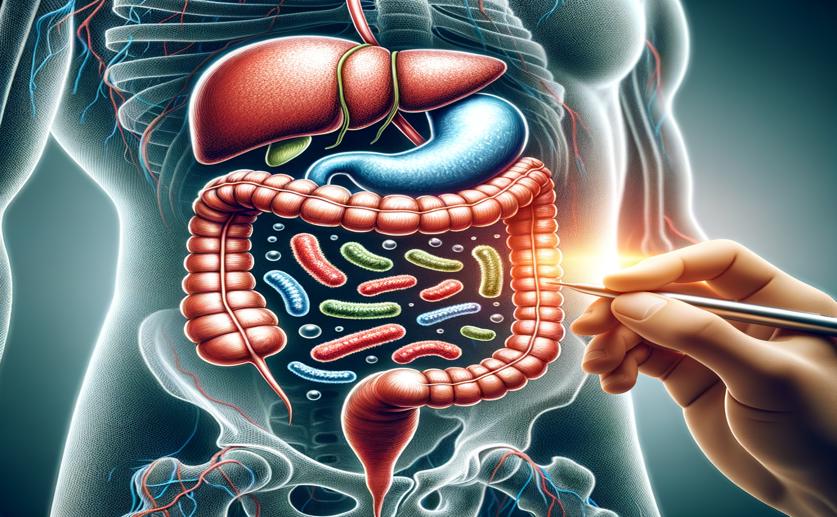
Image Source: Natural Science News, 2024
Key Findings
- The study by Nanjing Agricultural University explored the effects of the probiotic Bifidobacterium longum subsp. longum BL21 on chronic kidney disease (CKD) in rats
- BL21 significantly improved gut microbial populations, increasing microbial richness and beneficial bacteria
- The probiotic intervention reduced harmful uremic toxins in the blood, such as IS, IAA, and TMAO, in CKD rats
References
Main Study
1) Reduction in Serum Concentrations of Uremic Toxins Driven by Bifidobacterium Longum Subsp. Longum BL21 is Associated with Gut Microbiota Changes in a Rat Model of Chronic Kidney Disease
Published 3rd June, 2024
https://doi.org/10.1007/s12602-024-10293-5
Related Studies
2) Intestinal Dysbiosis, Barrier Dysfunction, and Bacterial Translocation Account for CKD-Related Systemic Inflammation.
3) Evaluation of the impact of gut microbiota on uremic solute accumulation by a CE-TOFMS-based metabolomics approach.
4) Role of the Gut Microbiome in Uremia: A Potential Therapeutic Target.



 31st May, 2024 | Greg Howard
31st May, 2024 | Greg Howard