
Understanding How Gamma-Terpinene Affects Cell Health and Blood Clotting
Jenn Hoskins
28th May, 2024
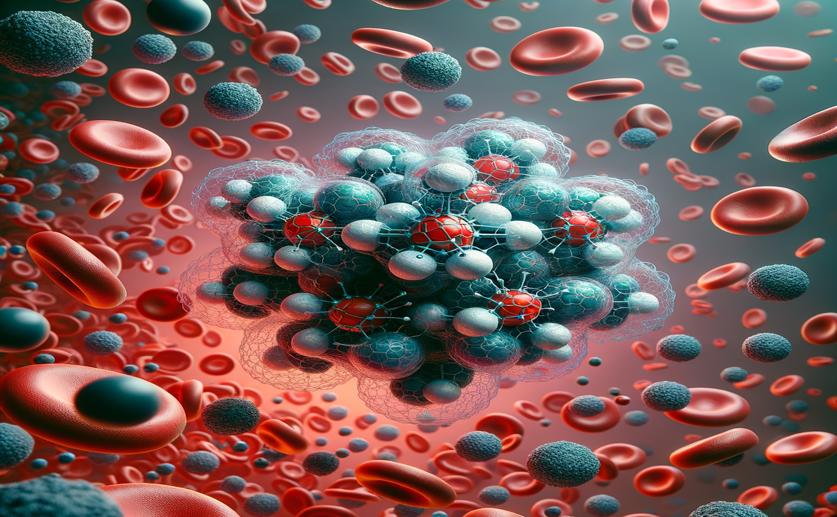
Image Source: Natural Science News, 2024
Key Findings
- The study by the Federal University of Piauí explored the potential of γ-TPN, found in essential oils, as a treatment for thromboembolic diseases
- γ-TPN showed good bioavailability and pharmacokinetics, indicating it could be effectively absorbed and utilized by the body
- γ-TPN significantly reduced platelet aggregation, suggesting it could help prevent blood clots without severe side effects
References
Main Study
1) Non-clinical investigations about cytotoxic and anti-platelet activities of gamma-terpinene.
Published 27th May, 2024
https://doi.org/10.1007/s00210-024-03173-w
Related Studies
2) Identification of a New Morpholine Scaffold as a P2Y12 Receptor Antagonist.
3) Role of ADP receptors on platelets in the growth of ovarian cancer.
4) Nucleoside triphosphates inhibit ADP, collagen, and epinephrine-induced platelet aggregation: role of P2Y₁ and P2Y₁₂ receptors.



 25th May, 2024 | Jim Crocker
25th May, 2024 | Jim Crocker