
How a Fungal Pathway Increases Drug Resistance
Jim Crocker
5th April, 2024
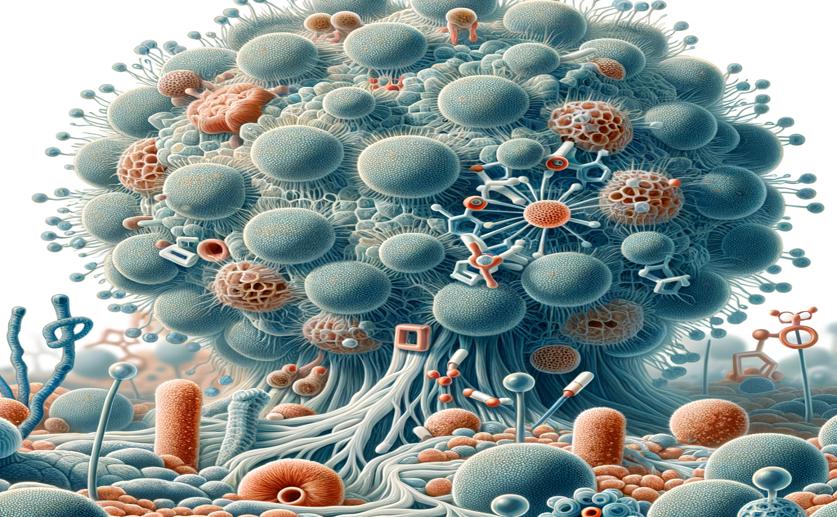
Image Source: Natural Science News, 2024
Key Findings
- Researchers at Musashino University found a gene in a fungus causing skin infections that contributes to drug resistance
- Deactivating this gene made the fungus more sensitive to the antifungal drug terbinafine
- A common acid reflux medication increased the effectiveness of terbinafine against resistant fungal strains
References
Main Study
1) The Ptk2-Pma1 pathway enhances tolerance to terbinafine in Trichophyton rubrum.
Published 3rd April, 2024
https://doi.org/10.1128/aac.01609-23
Related Studies
2) Discovery of Terbinafine Low Susceptibility Trichophyton rubrum strain in Japan.
3) Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine.
Journal: Antimicrobial agents and chemotherapy, Issue: Vol 49, Issue 7, Jul 2005
4) Clinical Trichophyton rubrum strain exhibiting primary resistance to terbinafine.
Journal: Antimicrobial agents and chemotherapy, Issue: Vol 47, Issue 1, Jan 2003



 16th January, 2024 | Jim Crocker
16th January, 2024 | Jim Crocker